Best Nursing School Bundle for Academic Excellence
Find out which best nursing school bundle ranks best for knowledge retention and test prep. Choose the right bundle for success.
Kullanıcılarına güvenli ortam sağlayan altyapısıyla Bettilt sektörde ön plandadır.
Kullanıcıların sisteme erişim için ilk durağı Bettilt adresidir.
Online bahislerde yüksek kazanç isteyenlerin tercihi her zaman güvenilir bahis siteleri olmuştur.
Her zaman kullanıcı odaklı düşünen Bettilt casino, basit kayıt süreci ve sade tasarımıyla yeni başlayanlar için idealdir.
Bahis sektöründe adından sıkça bettilt söz ettiren kaliteyi ön planda tutuyor.
Kazançlı kombinasyonlar hazırlamak isteyenler için bettilt analiz desteği sunar.
Türk bahis pazarının büyüme oranı bahsegel hoşgeldin bonusu yıllık %14 bu trendi yakından takip eder.
Accurate nursing dosage calculation is critical in patient care. A small mistake can lead to overdoses, underdoses or even life threatening situations. Studies show that “medication errors are among the most common healthcare mistakes, with dosage miscalculations being a significant factor” Institute of Medicine. This highlights the urgent need for nurses to master dosage calculations to ensure patient safety.
One common issue is misinterpreting drug orders. For example, confusing milligrams (mg) with micrograms (mcg) can result in a dangerously high dose. According to the National Patient Safety Foundation, “one extra zero in a dosage calculation can mean the difference between life and death.” Another frequent mistake is miscalculating pediatric doses as childrens weight based dosing requires precise calculations.
This nursing guide identifies the top 10 nursing dosage calculation errors and offers evidence based strategies to prevent them. These include double checking calculations, using standardized measurement tools and following the “Five Rights” of medication administration: right patient, right drug, right dose, right route and right time. As the American Nurses Association states, “A nurse’s vigilance in medication calculations is a key defense against errors in patient care.”
By understanding these common pitfalls and adopting best practices nurses can enhance medication safety, improve patient outcomes and strengthen their clinical skills. Let’s explore these critical errors and how to prevent them effectively.
Simple math mistakes can result in severe medication errors that affecting patient safety. Research from the American Journal of Nursing found that “17% of medication errors were due to miscalculations, often involving basic arithmetic mistakes,” says Smith. This highlights the importance of accuracy in dosage calculations.
Confusing milligrams (mg) with micrograms (mcg) or milliliters (mL) can lead to dangerous overdoses or ineffective underdoses. According to the Institute for Safe Medication Practices, “Medication errors due to unit conversion mistakes are among the most preventable causes of patient harm.” Nurses must be extra cautious with conversions especially in high risk drugs like insulin and opioids.
Unclear prescriptions whether handwritten or electronic can lead to serious nursing dosage calculation errors. A study by the Journal of Patient Safety found that “misinterpreted medication orders contribute to 15% of preventable drug errors.” Poor handwriting, abbreviations or unclear electronic entries make it easy for nurses to misread doses.
Adjusting dosages for patient-specific factors like age, weight, renal function and liver function is crucial. According to the Journal of Clinical Nursing, “25% of medication dosage errors occur because patient conditions are not properly considered.” For example, failing to adjust for kidney function when administering nephrotoxic drugs can lead to severe complications.
Applying the wrong formula especially in IV drug calculations can lead to severe medication errors. Research from the International Journal of Nursing Studies states, “Incorrect formula usage is a leading cause of infusion rate miscalculations that resulting in underdosing or overdosing.” Nurses must ensure they use the correct formulas for weight based dosing, IV flow rates and dilution calculations.
Rounding errors may seem minor but in nursing dosage calculation they can lead to significant dosing discrepancies especially in pediatric and IV drug administration. According to the Journal of Medication Safety “Even a slight rounding mistake in high risk drugs like insulin or anticoagulants can result in dangerous underdosing or overdosing.”
A misplaced decimal point can cause a tenfold overdose or underdose that putting patients at serious risk. The Institute for Safe Medication Practices warns, “One misplaced decimal can be the difference between therapeutic and toxic medication levels.” For example, writing 5.0 mg instead of 0.5 mg can lead to dangerous overdosing.
Incorrect IV flow rate calculations can result in underdosing or overdosing that affecting patient outcomes. According to the Journal of Nursing Practice. “Errors in IV medication rates can lead to serious complications, including toxicity or ineffective treatment.” Nurses must ensure precise calculations before administering IV medications.
Many medications have similar names that increasing the risk of administering the wrong drug. The Institute for Safe Medication Practices states, “Look alike, sound alike (LASA) medications are a major cause of preventable drug errors.” For example, DOBUTamine and DOPamine are commonly confused that leading to dangerous consequences.
While electronic medical records (EMRs) and smart pumps improve efficiency that they are not foolproof. System glitches, user errors or incorrect data entry can lead to medication mistakes. According to the Journal of Patient Safety, “Blindly trusting technology without manual verification increases the risk of medication errors.” Nurses must balance technology with critical thinking.
Errors in nursing dosage calculation can have serious consequences but with the right knowledge and practices they are preventable. As highlighted throughout this nursing guide that simple strategies like double checking calculations also using standardized tools and verifying medication orders with colleagues can greatly reduce the risk of errors. The Institute for Safe Medication Practices emphasizes, “Education and vigilance are key in preventing medication errors ensuring that patient safety remains a top priority.”
Mastering nursing dosage calculation requires nurses to be proactive that stay current with best practices and understand the unique needs of each patient. By calculating dosages carefully that confirming with second checks and using technology as a supplement not a replacement and nurses can avoid many common errors.
By embracing these evidence based strategies that nurses not only protect their patients but also foster a culture of safety and accountability. As the American Nurses Association states, “The vigilance and knowledge of nurses are essential in maintaining high standards of patient care.” Proper education, consistent practice and a commitment to safety are the foundation of reducing medication errors and ensuring that patients receive the right medication at the right time.
Find out which best nursing school bundle ranks best for knowledge retention and test prep. Choose the right bundle for success.
Complete nursing school workbook bundle! Includes flashcards for nursing students, cheat sheets, dosage calculation practice, and more.
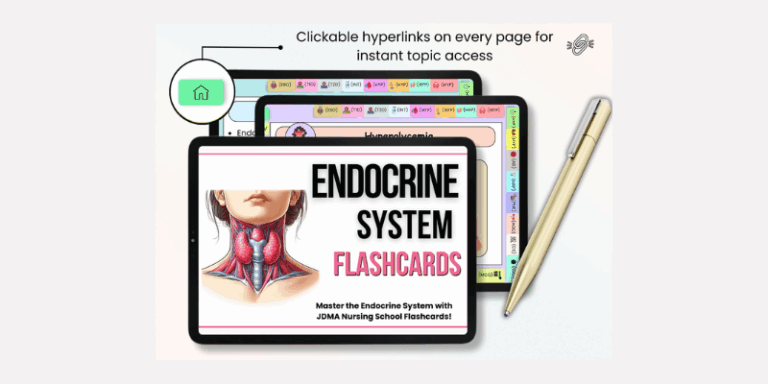
Master nursing concepts faster with our nursing school flashcards bundle! Printable & digital options for effective studying.
By subscribing to our newsletter you agree to our Terms and Conditions and Privacy Policy