Best Nursing School Bundle for Academic Excellence
Find out which best nursing school bundle ranks best for knowledge retention and test prep. Choose the right bundle for success.
Kullanıcılarına güvenli ortam sağlayan altyapısıyla Bettilt sektörde ön plandadır.
Kullanıcıların sisteme erişim için ilk durağı Bettilt adresidir.
Online bahislerde yüksek kazanç isteyenlerin tercihi her zaman güvenilir bahis siteleri olmuştur.
Her zaman kullanıcı odaklı düşünen Bettilt casino, basit kayıt süreci ve sade tasarımıyla yeni başlayanlar için idealdir.
Bahis sektöründe adından sıkça bettilt söz ettiren kaliteyi ön planda tutuyor.
Kazançlı kombinasyonlar hazırlamak isteyenler için bettilt analiz desteği sunar.
Türk bahis pazarının büyüme oranı bahsegel hoşgeldin bonusu yıllık %14 bu trendi yakından takip eder.
Medical surgical nursing plays a crucial role in healthcare. Focusing on caring for adult patients with a wide range of acute and chronic conditions. As this field evolves so too does the need for nurses to be proficient in managing complex care plans. Understanding diverse medical treatments. With advancements in healthcare continuous education is key medical surgical nursing course is now vital for nurses to grasp the intricate details of human medical surgical nursing. These courses provide a foundation for understanding diseases and treatments.Ensuring that nurses are well equipped to provide high quality care. The latest trends highlight the importance of integrating. These courses into nursing practice emphasizing the need for a comprehensive understanding of the human body to improve patient outcomes.
Medical surgical nursing is the backbone of healthcare handling a vast array of conditions and procedures. It is the largest specialty in nursing comprising nearly 50% of the U.S. nursing workforce according to the American Nurses Association (ANA). This field requires nurses to be versatile and skilled. Managing both acute and chronic medical conditions as well as pre and post operative care. The ability to care for patients across a wide range of medical scenarios makes medical surgical nursing essential to the healthcare system. Bridging gaps between different specialties and ensuring comprehensive patient care.
Dr. Rachel Anderson, a nursing educator emphasizes,
“The ability to care for patients across a wide range of medical conditions makes medical-surgical nursing a critical component of healthcare.”
This versatility not only allows nurses to support patients from diagnosis through recovery but also to adjust care plans as needed. The complexity of medical surgical nursing requires a deep understanding of anatomy, physiology and disease processes. Medical surgical courses are vital for providing this knowledge. Enabling nurses to deliver safe and effective care while navigating the challenges of diverse medical conditions. These courses ensure that nurses are prepared for the dynamic nature of their specialty. Helping to improve patient outcomes and reduce complications.
Medical surgical nursing education is evolving rapidly adapting to the demands of modern healthcare practice. As healthcare systems continue to advance so too must the methods used to train future nurses in this critical field. Here are three major trends shaping the education of medical surgical nurses: Simulation Based Learning, Blended Learning Approaches and the Use of Digital Health Records (EHRs).
Simulation is transforming how nursing students learn in medical surgical course. High fidelity simulators such as mannequins that can mimic real life patient. Responses like changes in heart rate or blood pressure allow students to practice clinical decision making, critical thinking and hands on skills in a safe controlled environment. According to a study published in the Journal of Nursing Education students. Who engage in simulation based learning techniques perform better in clinical settings and retain information longer with a reported 25% improvement in clinical decision making skills compared to traditional methods.
Example: Nursing schools often use high fidelity mannequins that can simulate real life scenarios such as respiratory distress, cardiac arrhythmias and seizures. These simulations enable students to experience a wide range of patient. Responses helping them build confidence and competence in managing complex situations without the risk of harming real patients. Through these simulations students can practice interventions, evaluate outcomes and refine their skills under supervision making it a vital tool for bridging the gap between theory and practice.
Blended learning combines online coursework with in person clinical rotations providing a flexible yet structured learning environment. This approach allows students to learn at their own pace accessing resources online to review concepts, videos and interactive modules. Then they apply these concepts in a clinical setting reinforcing their understanding through hands on experience. Research from the Journal of Advanced Nursing indicates that students in blended courses tend to score 10% higher on exams compared to those in traditional classroom settings. This model not only enhances theoretical knowledge but also builds practical skills in a real world context.
Benefit: Blended learning allows students to learn asynchronously. Enabling them to review complex topics multiple times before applying them in clinical practice. This method supports deeper understanding and critical thinking as students can revisit materials. When necessary and spend more time with challenging concepts. By merging online learning with hands on practice nursing students are better prepared to face the realities of medical surgical nursing where adaptability and quick decision making are crucial.
The integration of electronic health records (EHRs) into nursing curricula is essential for preparing students for real world nursing practice. Familiarity with EHR systems is critical for modern nurses as it allows them to manage patient data efficiently, document care and communicate effectively. With other healthcare professionals. A survey conducted by the American Medical Informatics Association found that 70% of nursing schools. Adopted EHR simulation as part of their medical surgical nursing courses. This trend reflects the growing importance of digital health technologies in healthcare. The need for nurses to be proficient in navigating these systems.
Impact: By incorporating EHR simulations students gain hands on experience with real world scenarios. Such as accessing patient records, entering notes and monitoring changes in patient status over time. This experience not only builds technical skills but also enhances critical thinking. As students must interpret data, make clinical decisions and collaborate with the healthcare team. The use of EHRs in nursing education ensures that graduates are well prepared for the technological landscape of modern healthcare. Where accurate documentation and communication are critical to patient safety and care continuity.
In conclusion these educational trends in medical surgical nursing highlight the need for a more integrated and adaptive approach to nurse training. By embracing simulation, blended learning. EHR use nursing schools are better preparing students for the complexities of real world practice. As healthcare continues to evolve these educational methods will remain vital in ensuring that nurses are equipped to provide high quality patient centered care in a rapidly changing environment.
Medical surgical nursing continues to evolve adapting to changes in healthcare delivery and patient needs. The latest trends in this field highlight a shift towards more personalized and technologically integrated care. From patient centered approaches to the use of telehealth and chronic disease management. These trends are shaping how nurses practice and how they are educated. Here’s an in depth look at these emerging practices and their impact on medical surgical nursing.
The shift towards patient centered care in medical surgical settings emphasizes a holistic and individualized approach to nursing. Nurses are no longer just care providers but also patient advocates. Ensuring that each patients unique needs and preferences are met. This approach considers not only the physical but also the emotional and social aspects of patient care. According to a study published in the International Journal of Nursing Studies patient centered care has been linked to improved patient satisfaction and faster recovery times. Dr. Emily Green, a clinical nurse specialist explains,
“Nurses are increasingly trained to be more than caregivers they are patient advocates, focusing on ensuring that each patient’s unique needs and preferences are addressed.“
The focus on individualized care plans allows nurses to provide more tailored interventions. Whether it is adjusting medication schedules for chronic pain management or coordinating support for patients undergoing major surgery. By understanding patients backgrounds, preferences and concerns. Nurses can provide more effective care enhancing both the quality of life and the treatment outcomes for their patients.
Telehealth has become an integral part of medical surgical nursing particularly following the COVID-19 pandemic. Remote monitoring allows nurses to keep track of patients conditions from afar facilitating timely interventions when necessary. This technology is not just a temporary solution but a permanent fixture in modern medical surgical practice. A study published in the Journal of Telemedicine and Telecare found that remote monitoring of chronic conditions reduced hospital readmissions by 30%. This reduction is significant considering the high costs associated with repeated hospital visits and the strain on healthcare resources.
Telehealth enables nurses to monitor vital signs, assess symptoms and adjust treatment plans based on real time data. This capability is crucial for managing chronic conditions such as diabetes, hypertension and heart disease. It allows for early detection of complications and quick intervention thereby preventing exacerbations that could lead to hospitalization. The COVID-19 pandemic accelerated the adoption of telehealth proving its effectiveness in maintaining continuity of care even when physical presence is not possible.
In medical surgical settings nurses are increasingly responsible for managing chronic diseases such as diabetes, hypertension and heart disease. This trend reflects the growing burden of chronic illness in the population and the need for effective ongoing care in medical surgical units. Programs that integrate chronic disease management. Medical surgical nursing education are becoming more common providing nurses with the knowledge and skills needed to monitor and manage these conditions. Courses like “Chronic Disease Management in Medical Surgical Nursing” focus on evidence based practices helping nurses stay updated on new treatment protocols and medications.
Continuous education is critical in this area. New treatments and technologies are frequently emerging requiring nurses to stay current with the latest developments. By incorporating chronic disease management into their practice. Nurses can not only provide better care but also educate patients on lifestyle changes, diet and medication adherence. This proactive approach helps prevent complications and hospital readmissions improving overall patient outcomes and quality of life.
The use of technology in patient education is becoming increasingly common in medical surgical nursing. Digital tools like videos, apps and websites are used to educate patients about their conditions and treatment plans. These tools provide patients with easy access to information helping them understand their health better and follow through with recommended treatments. A survey by the National Institute of Nursing Research found that patients who received digital education were more likely to understand their conditions and adhere to prescribed treatments. This is crucial in chronic disease management where adherence to medication and lifestyle changes is often a challenge.
Technology enhanced education also allows nurses to deliver information in a more personalized way. For example, a patient may watch a video on managing blood sugar levels for diabetes at their own pace or follow an app that reminds them when to take their medication. This personalized approach can lead to better engagement, improved outcomes and greater satisfaction with care. By integrating these technologies into their practice medical surgical nurses can empower patients to take an active role in their health leading to better long term outcomes.
In conclusion, these trends in medical surgical nursing practice reflect a move towards more patient centered technology driven care. As the healthcare landscape continues to change these practices will be essential in ensuring that nurses are equipped to meet the complex needs of their patients. Through ongoing education and adaptation to new technologies, medical surgical nurses are prepared to provide high quality care in an increasingly demanding environment.
While the trends in medical surgical nursing such as simulationbased learning, telehealth and chronic disease management. Offer significant benefits they also present several challenges that can impact their effective implementation and integration into practice. These challenges stem from time constraints, resistance to change and a lack of resources. Understanding these obstacles is crucial for developing strategies to overcome them and ensure that nurses can fully benefit from these advances.
One of the major challenges in adapting to new trends in medical surgical nursing is the issue of time. Nurses often face heavy workloads making it difficult to dedicate sufficient time to continuous learning and practice. The demands of patient care, administrative responsibilities and clinical rotations can leave little room for extra training. Such as participating in simulation sessions or keeping up with the latest research and technologies. According to a study in the Journal of Continuing Education in Nursing time constraints are a significant barrier to implementing simulation based learning effectively as nurses struggle to balance their schedules with these additional learning opportunities. Dr. Emily Green, a clinical nurse specialist notes,
“Even with the best intentions many nurses find it challenging to fit in the time required for new methods like simulation or EHR training given their already packed days.”
Another significant challenge is resistance to change among healthcare professionals. Some nurses and healthcare providers are slow to adopt new technologies or methods. Which can hinder their integration into medical surgical nursing practice. This resistance can be rooted in fear of the unknown lack of confidence in using new technologies or simple inertia. The COVID-19 pandemic while accelerating the adoption of telehealth also highlighted these challenges. A survey published in the Nursing Outlook journal found that many nurses still prefer traditional methods of patient care over newer technology driven approaches. This resistance can affect not only the integration of digital health records and telehealth but also the broader adoption of patient centered or care practices.
Many nursing schools and healthcare facilities lack the resources to implement simulation based learning or digital health records effectively. This gap is particularly pronounced in smaller or rural settings where budgets may be limited and access to advanced technologies is restricted. The International Journal of Nursing Education reports that only a small percentage of nursing schools have the necessary equipment and funding to provide high fidelity simulations for their students. This lack of resources can make it difficult for nursing students to gain hands on experience with digital tools and technologies which are increasingly essential in modern practice. The impact of this limitation is clear without adequate training nurses may feel ill prepared to handle complex patient scenarios and the technological demands of their roles.
In conclusion, while the trends in medical surgical nursing education and practice are designed to improve patient outcomes and prepare nurses because the complexities of the field challenges such as time constraints, resistance to change and a lack of resources can impede their effective implementation. Addressing these challenges requires a concerted effort from nursing schools, healthcare organizations and policymakers to provide the necessary support and training. By overcoming these barriers medical surgical nurses can better integrate these advances into their practice ultimately improving patient care and outcomes.
The landscape of medical surgical nursing education and practice is rapidly changing. By integrating simulation based learning, digital tools and a strong emphasis on patient centered care nurses are better equipped to meet the complex challenges of this field. Dr. Anderson highlights,
“Adapting to these changes is not just about keeping up with technology it is about enhancing patient care through informed skilled nursing practice.”
For both students and practicing nurses staying informed about these emerging trends that is essential for maintaining excellence in medical surgical nursing. By continuously updating their knowledge and skills nurses can provide the highest level of care and effectively navigate the evolving healthcare environment.
Find out which best nursing school bundle ranks best for knowledge retention and test prep. Choose the right bundle for success.
Complete nursing school workbook bundle! Includes flashcards for nursing students, cheat sheets, dosage calculation practice, and more.
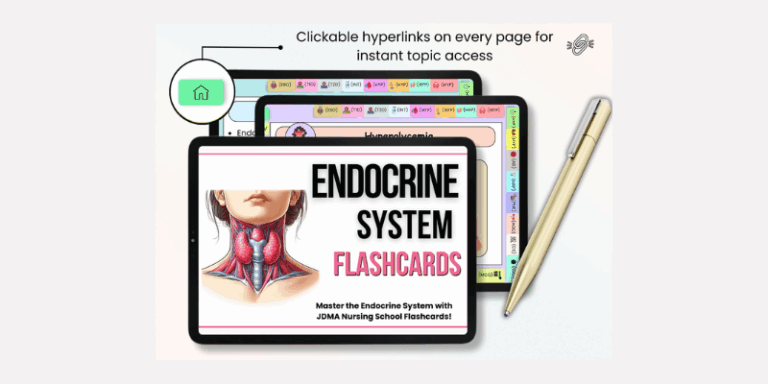
Master nursing concepts faster with our nursing school flashcards bundle! Printable & digital options for effective studying.
By subscribing to our newsletter you agree to our Terms and Conditions and Privacy Policy